Your ‘Stressed’ Feeling That Might Be a Magnesium Deficit
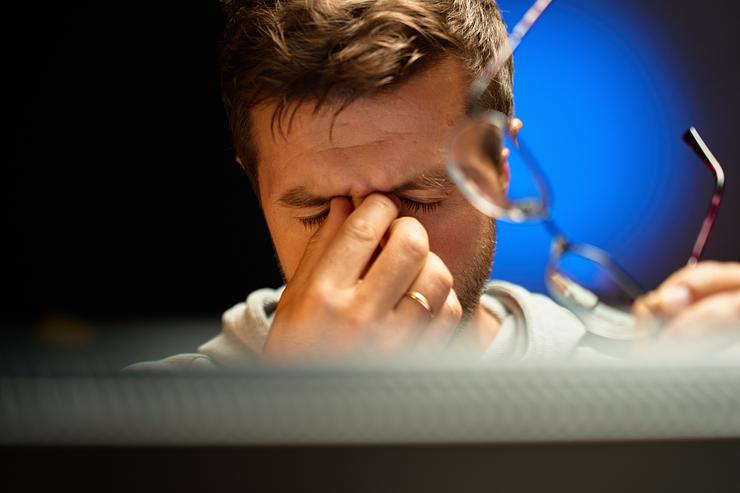
You know that feeling where your body is technically fine, but you don’t feel fine. Your chest feels tight for no reason. Your shoulders live up near your ears. Your jaw keeps clenching. Your mind won’t stop running even when you’re exhausted. You’re tired, but you can’t fully relax. You’re calm on the outside, but your nervous system feels like it’s buzzing.
Most people label that feeling as stress. And sometimes it is. Life is demanding, work is relentless, and modern living constantly keeps your brain switched on. But sometimes, that “stressed” feeling is also your body quietly missing something basic. Magnesium.
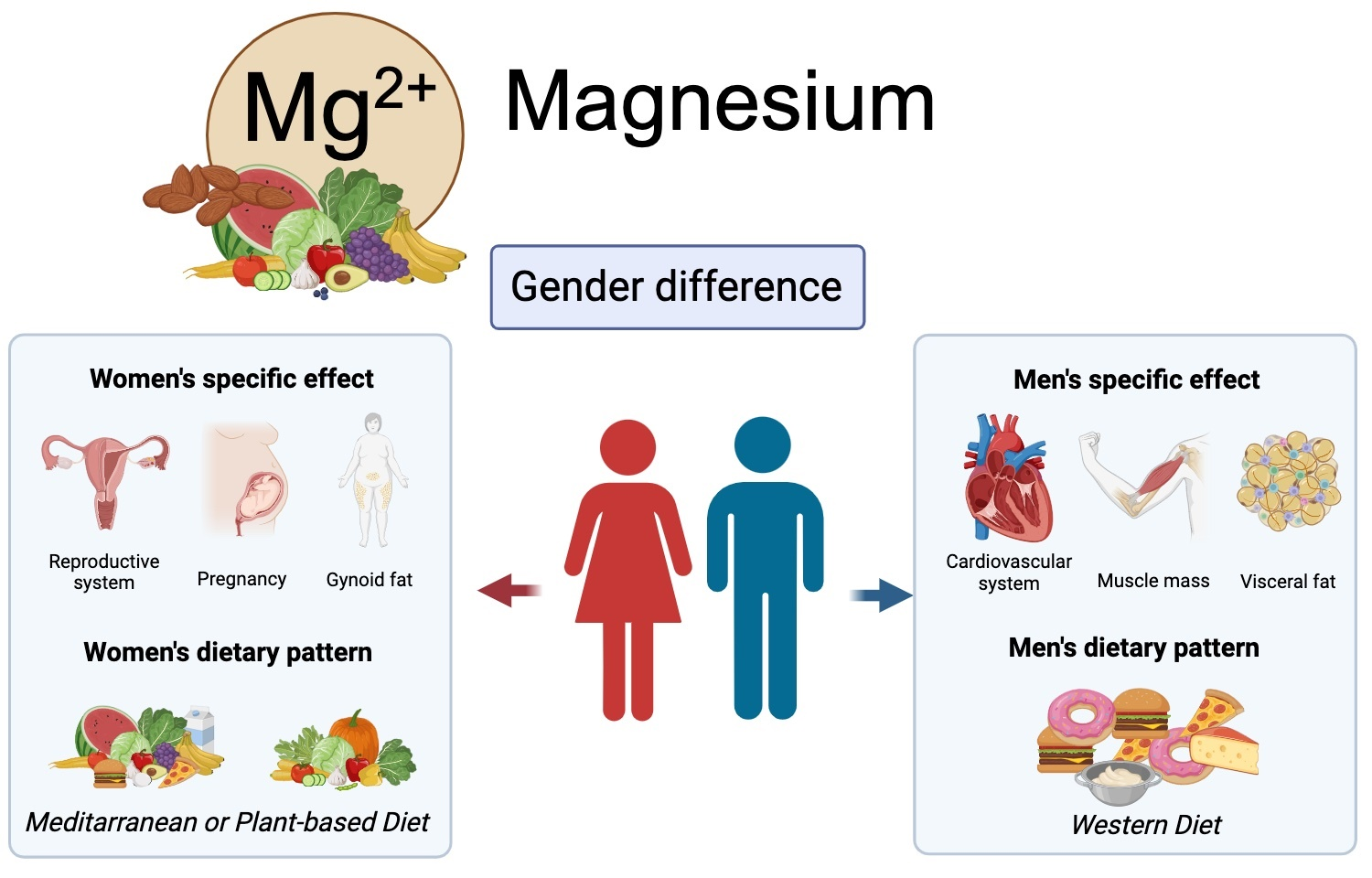
Not in a trendy “take this supplement and fix your life” way. In a simple biological way. Magnesium is involved in hundreds of processes in the body, including nervous system regulation, muscle relaxation, and sleep quality. When your intake is low, your stress response can feel louder and your ability to come down from stress can feel weaker. And because magnesium deficiency can be subtle, many people walk around feeling tense and restless without realizing there’s a nutritional piece to the puzzle.
Magnesium is a nervous system mineral, not just a “supplement”
Magnesium often gets marketed like a sleep hack. But the truth is, it’s foundational. Magnesium is required for normal nerve function, muscle function, and energy metabolism. It also plays a role in how your body responds to stress.
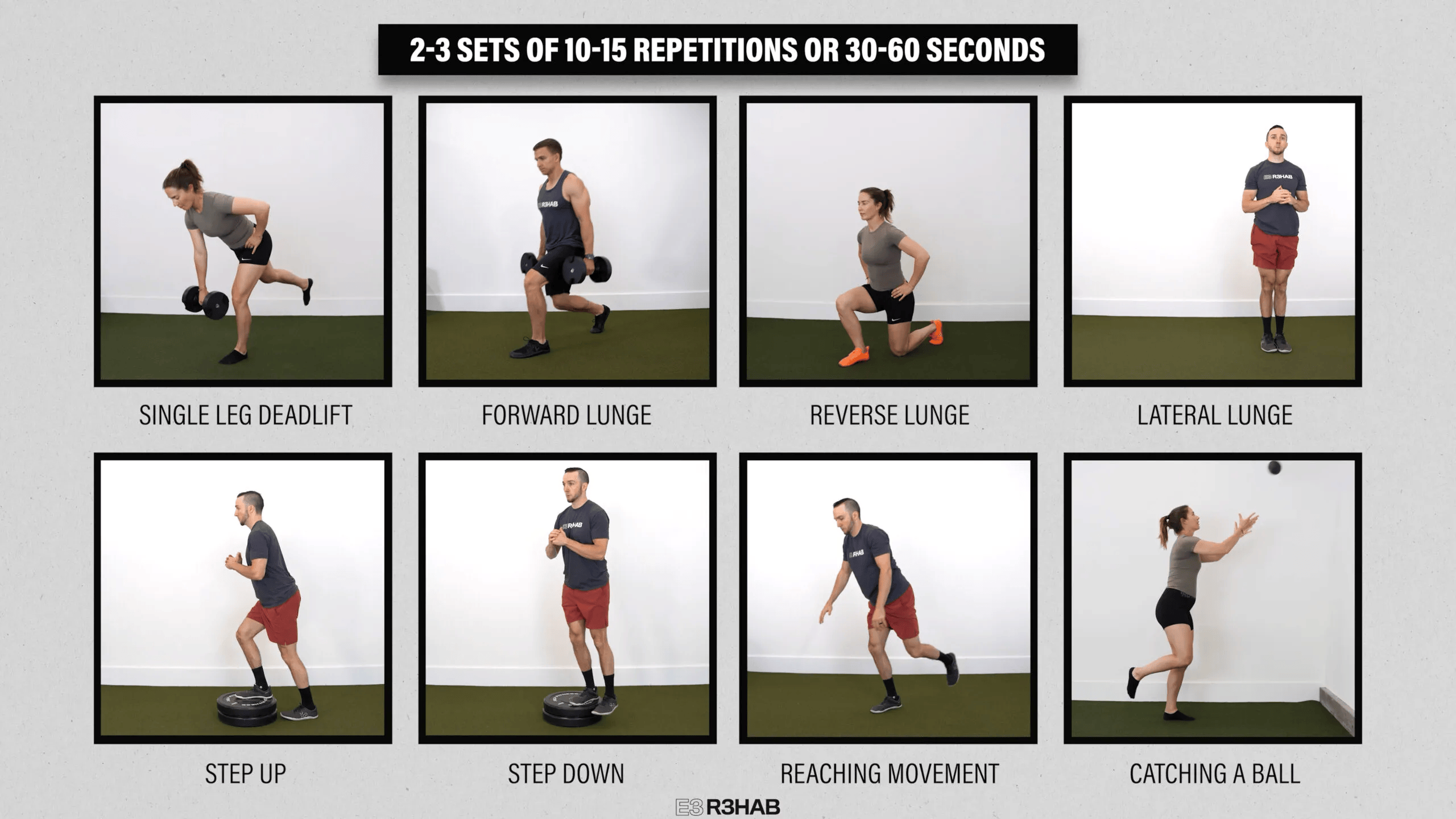
Your nervous system has two modes: “go” and “slow down.” Stress pushes you into “go.” Magnesium helps support the “slow down” side, partly by influencing neurotransmitter activity and helping muscles relax after contraction.
So if you’re living in a high stress environment and your magnesium intake is low, your body can feel like it’s stuck in the on position.
Not because you’re dramatic. Because your system doesn’t have the raw materials to regulate itself smoothly.

The modern lifestyle quietly burns through magnesium
Magnesium is easy to miss because the foods that contain it are often the foods people eat less of when life gets busy.
Leafy greens. Beans. Lentils. Nuts. Seeds. Whole grains. Dark chocolate. Avocado.
When stress rises, most people shift toward convenience foods. More refined carbs. More packaged meals. More sugar. Less variety. Less fiber. Less mineral density.
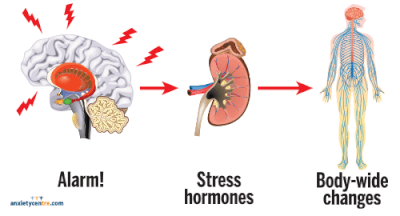
At the same time, stress itself may increase magnesium losses. Chronic stress can influence magnesium status through hormonal and metabolic pathways, which is why magnesium is often discussed in relation to stress physiology (Galland 1992).
This creates a loop that’s easy to fall into. You feel stressed, so you eat more processed foods. Your magnesium intake drops. Your nervous system feels more reactive. You feel even more stressed.
And because the symptoms are vague, you assume it’s just your personality or your workload.
Why magnesium affects sleep and “wired tired” energy
One of the most frustrating feelings is being exhausted but unable to sleep.
You get into bed and your brain starts sprinting. Or you fall asleep but wake up at 3am with a racing mind. Or you sleep but wake up feeling like you never fully powered down.
Magnesium supports sleep partly through its role in nervous system regulation and its interaction with neurotransmitters involved in relaxation. In research, magnesium supplementation has been studied for sleep quality, especially in older adults, with some evidence of benefit (Abbasi et al. 2012).
This doesn’t mean magnesium is a magic pill for insomnia. But if your sleep is fragile and your stress is high, magnesium can be one of the missing pieces that makes it easier for your body to shift into rest mode.
Magnesium also supports your stress response, not just your mood
When people talk about “stress,” they usually mean thoughts and emotions.
But stress is also physical. It’s your heart rate. Your muscle tone. Your breathing pattern. Your gut motility. Your blood sugar stability. Your nervous system readiness.
Magnesium plays roles across many of these systems. It’s involved in energy production, and it supports normal muscle and nerve function. When magnesium is low, your stress response can feel sharper because your baseline is already strained.
Some research suggests magnesium may influence the hypothalamic pituitary adrenal axis, which is a major stress regulation system in the body (Galland 1992). Again, not a miracle cure, but a meaningful lever.
This is why magnesium deficiency can look like anxiety, even when the real issue is your body struggling to regulate.
Before you supplement, check the basics
A lot of people jump straight to supplements because it feels faster. But if you can raise magnesium intake through food, you get additional benefits that supplements don’t provide, like fiber, potassium, antioxidants, and better overall diet quality.
If you want to build a magnesium supportive day of eating, it can be simple:
Add a handful of nuts or seeds daily. Pumpkin seeds are especially magnesium rich.
Eat beans or lentils a few times per week.
Include leafy greens regularly, even in small amounts.
Choose whole grains sometimes instead of refined grains.
Add cacao or dark chocolate intentionally, not as a stress binge.
Even one or two small changes can shift your baseline.
This matters because many people don’t have one giant deficiency. They have a long term pattern of being slightly low on key nutrients, while living in a high demand environment. That mismatch adds up.
If you do supplement, it’s about consistency and type
If you decide to supplement, it’s worth knowing that not all magnesium forms are the same. Some forms are better tolerated and better absorbed than others. Magnesium glycinate is often used for relaxation because it tends to be gentle on the stomach. Magnesium citrate can be helpful but may have a laxative effect for some people. Magnesium oxide is common and cheap but generally less bioavailable.
The goal is not to take the highest dose possible. The goal is to support your baseline without creating digestive issues.
The NIH provides clear guidance on recommended intakes and upper limits for supplemental magnesium, and it’s worth staying within those ranges unless you’re working with a clinician (NIH Office of Dietary Supplements 2022).
If you have kidney disease or take medications that affect electrolytes, you should not self prescribe magnesium without medical guidance.
The takeaway
Not every stressed feeling is a magnesium problem.
But if you’re constantly tense, restless, sleeping poorly, and feeling like your nervous system is stuck in overdrive, magnesium is worth considering. It supports normal nerve and muscle function, helps the body downshift into relaxation, and may improve sleep quality when intake is low.
The best part is that this is not an extreme intervention. It’s a simple return to basics. More mineral dense foods, more consistent recovery, and less forcing your body to run on empty.
Sometimes the fastest way to feel calmer isn’t more productivity hacks.
It’s giving your nervous system what it needs to actually relax.
References
Abbasi, B, Kimiagar, M, Sadeghniiat, K, Shirazi, MM, Hedayati, M and Rashidkhani, B 2012, ‘The effect of magnesium supplementation on primary insomnia in elderly: a double blind placebo controlled clinical trial’, Journal of Research in Medical Sciences, vol. 17, no. 12, pp. 1161–1169, viewed 21 January 2026, https://pubmed.ncbi.nlm.nih.gov/23853635/.
Galland, L 1992, ‘Magnesium and immune function: an overview’, Magnesium and Trace Elements, vol. 10, no. 2–4, pp. 167–173, viewed 21 January 2026, https://pubmed.ncbi.nlm.nih.gov/1844561/.
NIH Office of Dietary Supplements 2022, Magnesium Fact Sheet for Health Professionals, viewed 21 January 2026, National Institutes of Health, https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/.